By Farah Madhat, PharmD, EVP, Innovation and Experience
Pharmacy deserts, or areas where individuals lack convenient, reliable access to pharmacy services1, are a growing concern with serious implications for patients managing complex health conditions. For millions of Americans, strong connectivity to pharmacy services is essential to ensure the safe and effective use of medications, leading to improved quality of life, longevity, and more efficient healthcare utilization.
Frequently defined as census tracts without pharmacies within one mile in urban areas or within ten miles in rural areas, pharmacy deserts pose heightened risks for individuals managing multiple chronic conditions.2 For these patients, treatment success often depends on the inclusion of pharmacist interventions that promote adherence, surveillance for drug interactions, and optimization of regimens as needs evolve.3 As pharmacy closures continue to accelerate, this vital layer of care coordination begins to disappear.
Today, an estimated 57.1 million individuals (17.7% of the U.S. population) live in pharmacy deserts, spanning all 50 states.1 This stark landscape reveals a critical need to strengthen pharmacy care delivery for patients with complex therapeutic needs. For health plans serving especially complex, polychronic populations, such as Dual-Eligible and Chronic Condition Special Needs Plans (D-SNPs and C-SNPs), these challenges present clear opportunities to improve outcomes for vulnerable patients through accessible pharmacy services delivered in home- and community-based settings.
Pharmacy Closures Amid Rising Demand for Care
Between 2010 and 2021, nearly 30% of the retail pharmacies operating in the U.S. closed, amounting to more than 26,000 stores.4 This contraction in pharmacy infrastructure has left entire communities without essential access points for healthcare services. As these physical resources diminish, patients face growing barriers to obtaining medications, maintaining adherence, and staying connected to essential care.
For those managing multiple medications across complex conditions, the loss of accessible pharmacy services compounds these challenges, raising the likelihood of medication-related risks, harms, and adverse outcomes.5
These patterns are mirrored in national public health data. Adverse Drug Events (ADEs), defined as harm resulting from medication use, are now the third leading cause of death in the U.S., surpassed only by heart disease and cancer.6 In response, the American Society of Pharmacovigilance was compelled to rebrand its public awareness campaign from “Fourth Cause” to “Third Cause,” acknowledging the rising mortality rates stemming from medication-related problems. Financially, the impact is no less significant: an estimated $528 billion in annual health expenditures are attributed to unoptimized or poorly coordinated medication therapy.7
For SNPs, the national rise in ADEs underscores the importance of integrating comprehensive pharmacy services into broader population health strategies to improve quality and cost outcomes.
Implications for Dual-Eligible Populations and SNP Performance
Enrollment in SNPs has expanded dramatically in recent years, tripling between 2018 and 2024 from 2.6 million to 7.3 million members. Much of that growth has been concentrated in Dual-Eligible SNPs: over the same period, D-SNP enrollment rose from 2.2 million to 5.8 million. SNPs now represent roughly one in five Medicare Advantage enrollees, signaling their growing influence on complex care delivery and management.8
Dual-eligible members are also among the most clinically complex. They often contend with high medication burden, multiple prescribers, functional limitations, and transportation barriers.9 For D-SNP and C-SNP plans, managing these populations becomes increasingly difficult and consequential as the pharmacy landscape continues to evolve.
Without a strong pharmacy partner, SNPs can struggle to preserve quality and safety performance, as well as cost containment amid rising rates of overutilization.10 Establishing such a partnership lays the foundation for scalable, measurable plan improvement to better serve high-need, polychronic populations.
Redesigning Access: Demonstrated Impact in Dual-Eligible Populations
To address these challenges, enhanced pharmacy models are extending care beyond the confines of traditional brick-and-mortar establishments. By integrating clinical pharmacist support with home delivery, adherence packaging, and virtual engagement, these models reestablish continuity for members with unique medication challenges, particularly dual-eligible patients.
Independent claims analysis evaluated AnewHealth’s high-touch, at-home pharmacy model for dual-eligible members with multiple chronic conditions and complex medication regimens. Using three years of retrospective claims data and 1:1 propensity matching, the third-party validated study compared outcomes for members supported by AnewHealth with those using other pharmacies.
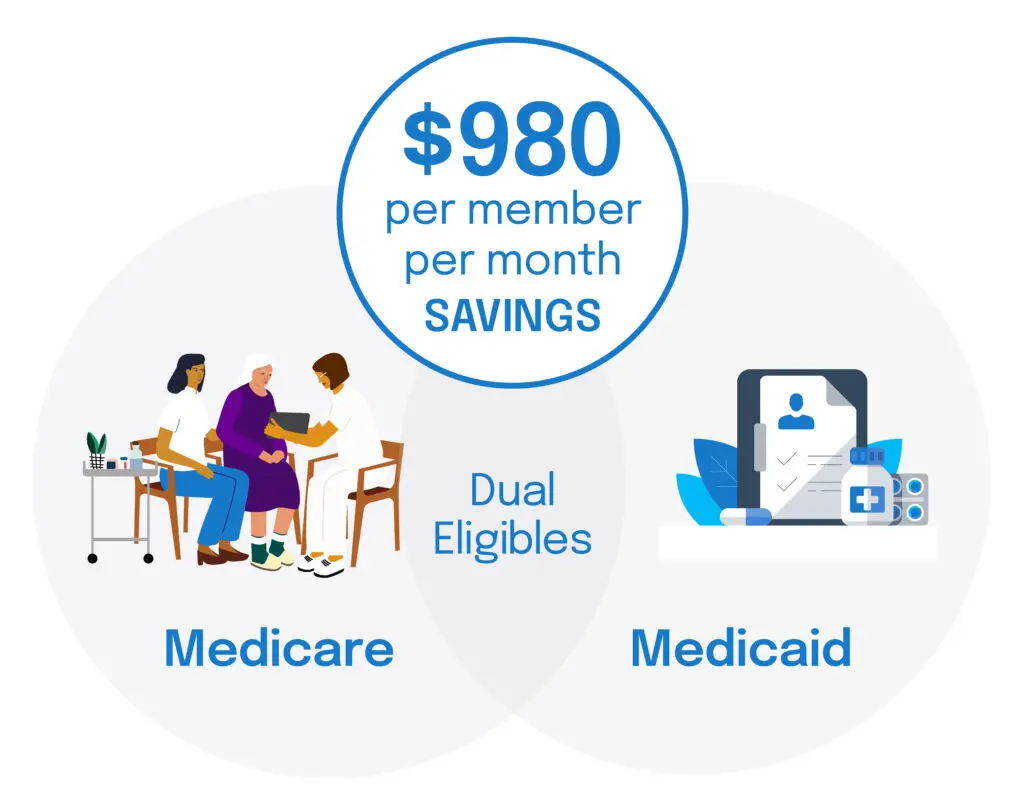
The analysis found that dual-eligible members supported by AnewHealth achieved $980 in per member per month savings compared to matched peers. These savings were driven by an omnichannel, pharmacy-at-home model that resolves critical care gaps typically exacerbated by pharmacy deserts, ensuring consistent access to care, clinical oversight, and adherence support. By maintaining safer, more effective medication regimens, members experienced fewer hospitalizations and emergency visits, along with a meaningful reduction in total cost of care.11
Conclusion
Pharmacy deserts represent a dangerous divide between the needs of polychronic patients and the healthcare system’s ability to support them.
Pharmacist-led, integrated models that extend care into the home are redefining what medication management can achieve. Enhanced services deployed through these models offer the access, coordination, and clinical engagement that traditional pharmacy models cannot sustain.
For D-SNPs and C-SNPs, aligning with a pharmacy partner built to serve complex populations can drive measurable improvement in quality, safety, and cost outcomes among their most vulnerable populations.
¹ Mathis WS, Berenbrok LA, Kahn PA, Appolon G, Tang S, Hernandez I. Vulnerability Index Approach to Identify Pharmacy Deserts and Keystone Pharmacies. JAMA Netw Open. 2025;8(3):e250715. doi:10.1001/jamanetworkopen.2025.0715
² Qato DM, Daviglus ML, Wilder J, Lee T, Qato D, Lambert B. ‘Pharmacy deserts’ are prevalent in Chicago’s predominantly minority communities, raising medication access concerns. Health Aff (Millwood). 2014;33(11):1958-1965. doi:10.1377/hlthaff.2013.1397
³ Stein A, Finnel S, Bankes D, Jin H, Awadalla MS, Johnson J, Turgeon J. Health outcomes from an innovative enhanced medication therapy management model. Am J Manag Care. 2021;27(suppl 16):S300-S308. https://doi.org/10.37765/ajmc.2021.88755
⁴ Guadamuz JS, Alexander GC, Kanter GP, Qato DM. More US pharmacies closed than opened in 2018–21; independent pharmacies, those in Black, Latinx communities most at risk. Health Aff (Millwood). 2024;43(12):In Press. https://doi.org/10.1377/hlthaff.2024.00192
⁵ Michaud V, Smith MK, Bikmetov R, Dow P, Johnson J, Stein A, Finnel S, Jin H, Turgeon J. Association of the MedWise Risk Score with health care outcomes. Am J Manag Care. 2021;27(suppl 16):S280-S291. https://doi.org/10.37765/ajmc.2021.88753
⁶ American Society of Pharmacovigilance. Predicting adverse drug event prevalence: A data-driven approach. StopADR. Published March, 2025. https://stopadr.org/blog/predicting-adverse-drug-event-prevalence-a-data-driven-approach
⁷ Watanabe JH, McInnis T, Hirsch JD. Cost of Prescription Drug-Related Morbidity and Mortality. Ann Pharmacother. 2018 Sep;52(9):829-837. doi: 10.1177/1060028018765159. Epub 2018 Mar 26. PMID: 29577766.
8 A closer look at the growing role of Special Needs Plans in Medicare Advantage. KFF. Published September 25, 2024. kff.org/medicare/a-closer-look-at-the-growing-role-of-special-needs-plans-in-medicare-advantage/
9 10 Things to Know About Medicare Advantage Dual-Eligible Special Needs Plans (D-SNPs). KFF. Published February 9, 2024. kff.org/medicare/10-things-to-know-about-medicare-advantage-dual-eligible-special-needs-plans-d-snps/
10 Keohane LM, Tummarakota S. Publicly Reported Quality Performance for Dual-eligible Special Needs Plans, 2010-2019. J Aging Soc Policy. 2023 Jun 22:1-21. doi: 10.1080/08959420.2023.2226309. Epub ahead of print. PMID: 37348455; PMCID: PMC10739605.
11 Driving Savings in Total Cost of Care: How a High-Touch Medication Management Program Drives Significant Savings for Complex Members. anewhealthrx.com/capabilities/end-to-end-pharmacy-care-management/



